Syndrome Description
Learn more about M-CM
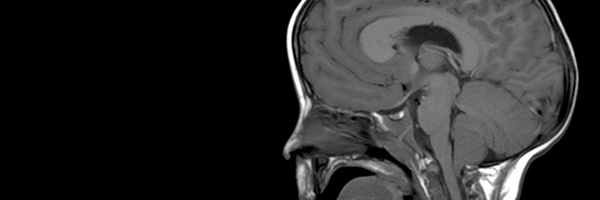
Newly published management guidelines call for a baseline brain and spine MRI at time of diagnosis, then every 6 months from 0-2 years and every year from 2-6 years with more frequent imaging if particular concerns arise. By age six, the rapid increase in head circumference has slowed and the concerns with the growth of the cerebellum decrease. Imaging beyond age 6 years should depend on previous findings and clinical course.
While hydrocephalus is commonly seen in M-CM, placing a ventriculperitoneal (VP) shunt does not completely correct the macrocephaly in affected individuals because the primary cause of macrocephaly in M-CM is brain overgrowth. It may reduce the degree of macrocephaly and may over time slow the rate in which the head enlarges in some, but not all affected individuals. Some have also treated hydrocephalus successfully with an endoscopic third ventriculostomy (ETV). This procedure eliminates the need for placement of foreign objects such as the tubing required in VP shunting, thus theoretically reducing complications after surgery. However, there is no clear consensus on the best surgical treatment for hydrocephalus in M-CM. M-CM patients with both ETV and VP shunt have required revisions.

When extreme brain overgrowth and CTH cause symptoms of brainstem compression, some M-CM patients have been successfully treated with a procedure called a posterior fossa decompression. This procedure surgically enlarges the opening at the base of the skull, allowing the cerebellum to grow in a space that can now accommodate its size. The goal of this procedure is to resolve or prevent symptoms due to brainstem compression.
The presence of CTH increases the risk of syringomyelia, a condition where a cyst, called a syrinx, forms on the spinal cord. A syrinx can be detected via spinal MRI. This condition requires monitoring and sometimes surgical management.
Many individuals who have CTH, an overgrown cerebellum, and enlarged ventricles will require neurosurgery at some point. The timing and type of intervention is a delicate matter and is best determined on a case-by-case basis. Neurosurgical options are dependent upon a number of factors including the severity of the brain abnormalities, the opinions of physicians directly involved in that person’s care as well as symptoms.
Order brochures or download a PDF
Guidelines from published research literature
Guidance for clinical genetic testing

Explore the results of a patient survey conducted in 2012

Explore the research literature related to M-CM

An extensive list of resources